|
Virgin and Child, Enthroned, The Master of Moulins, 1499 |
ADULT
STEM
CELLS
in CLINICAL
PRACTICE:
|
|
|
Virgin and Child, Enthroned, The Master of Moulins, 1499 |
ADULT
STEM
CELLS
in CLINICAL
PRACTICE:
|
|
Lancet. Volume 364 Issue 9436 Page 766
|
|
 |
|
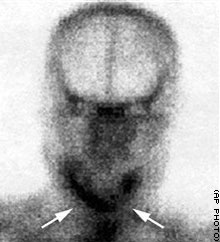
Arrows show a titanium cage, in which patient’s new jaw was grown, implanted under his shoulder blade. |
CT scan shows jaw in place. The jaw has shown continued bone growth after the transplant. Patient ate bread and sausages in hospital. |
LANCET ABSTRACT:
BACKGROUND: A major goal of research in bone transplantation is the ability to avoid creation of secondary bone defects. We aimed to repair an extended mandibular discontinuity defect by growth of a custom bone transplant inside the latissimus dorsi muscle of an adult male patient.
METHODS: Three-dimensional computed tomography (CT) scanning and computer-aided design techniques were used to produce an ideal virtual replacement for the mandibular defect. These data were used to create a titanium mesh cage that was filled with bone mineral blocks and infiltrated with 7 mg recombinant human bone morphogenetic protein 7 and 20 ml of the patient's bone marrow. Thus prepared, the transplant was implanted into the latissimus dorsi muscle and 7 weeks later transplanted as a free bone-muscle flap to repair the mandibular defect.
FINDINGS: In-vivo skeletal scintigraphy showed bone remodelling and mineralisation inside the mandibular transplant both before and after transplantation. CT provided radiological evidence of new bone formation. Postoperatively, the patient had an improved degree of mastication and was satisfied with the aesthetic outcome of the procedure.
INTERPRETATION: Heterotopic bone induction to form a mandibular replacement inside the latissimus dorsi muscle in a human being is possible. This technique allows for a lower operative burden compared with conventional techniques by avoiding creation of a secondary bone defect. It also provides a good three-dimensional outcome.
Doctors grow new jaw in man’s back CNN.com
Saturday, August 28, 2004 Posted: 8:57 AM EDT (1257 GMT)
CNN article. LONDON, England (AP) -- A German who had his lower jaw cut out because of cancer has enjoyed his first meal in nine years -- a bratwurst sandwich -- after surgeons grew a new jaw bone in his back muscle and transplanted it to his mouth in what experts call an “ambitious’’ experiment. [
Growth and transplantation of a custom vascularised bone graft in a man P H Warnke, I N G Springer, J Wiltfang, Y Acil, H Eufinger, M Wehmöller, P A J Russo, H Bolte, E Sherry, E Behrens, H Terheyden Lancet, Volume 364 Issue 9436 Page 766
According to this week’s issue of The Lancet medical journal, the German doctors used a mesh cage, a growth chemical and the patient’s own bone marrow, containing stem cells, to create a new jaw bone that fit exactly into the gap left by the cancer surgery.
Tests have not been done yet to verify whether the bone was created by the blank-slate stem cells and it is too early to tell whether the jaw will function normally in the long term.
But the operation is the first published report of a whole bone being engineered and incubated inside a patient’s body and transplanted.
Stem cells are the master cells of the body that go on to become every tissue in the body. They are a hot area of research with scientists trying to find ways to prompt them to make desired tissues, and perhaps organs.
But while researchers debate whether the technique resulted in a scientific advance involving stem cells, the operation has achieved its purpose and changed a life, said Stan Gronthos, a stem cell expert at the Institute of Medical and Veterinary Science in Adelaide, Australia.
“A patient who had previously lost his mandible (lower jaw) through the result of a destructive tumor can now sit down and chew his first solid meals in nine years ... resulting in an improved quality of life,’’ said Gronthos, who was not connected with the experiment.
The operation was done by Dr. Patrick Warnke, a reconstructive facial surgeon at the University of Kiel in Germany. The patient, a 56-year-old man, had his lower jaw and half his tongue cut out almost a decade ago after getting mouth cancer. Since then, he had only been able to slurp soft food or soup from a spoon.
In similar cases, doctors can sometimes replace a lost jawbone by cutting out a piece of bone from the lower leg or from the hip and chiseling it to fit into the mouth.
This patient could not have that procedure because he was taking a potent blood thinner for another condition and doctors considered it too dangerous to harvest bone from elsewhere in his body since extraction leaves a hole where the bone is taken, creating an extra risk of bleeding.
Artificial jaws made from plastic or other materials are not used because they pose too much of a risk of infection.
“He demanded reconstruction,’’ Warnke said. “This patient was really sick of living.’’
Warnke and his group began by creating a virtual jaw on a computer, after making a three-dimensional scan of the patient’s mouth.
The information was used to create a thin titanium micro-mesh cage. Several cow-derived pure bone mineral blocks the size of sugar lumps where then put inside the structure, along with a human growth factor that builds bone and a large squirt of blood extracted from the man’s bone marrow, which contains stem cells.
The surgeons then implanted the mesh cage and its contents into the muscle below the patient’s right shoulder blade. He was given no drugs, other than routine antibiotics to prevent infection from the surgery.
The implant was left in for seven weeks, when scans showed new bone formation. It was removed about eight weeks ago, along with some surrounding muscle and blood vessels, put in the man’s mouth and connected to the blood vessels in his neck.
Scans showed new bone continued to form after the transplant.
Four weeks after the operation, the man ate a German sausage sandwich, his first real meal in nine years. He eats steak now, but complains to his doctor that because he has no teeth he has to cut it into such small pieces that by the time he gets to the end of the steak, it’s cold.
He has reported no pain or any other difficulties associated with the transplant, Warnke said, adding that he hopes to be able to remove the mesh and implant teeth in the new jaw about a year from now.
Paul Brown, head of the Center for Tissue Regeneration Science at University College in London, said it’s not clear any major scientific ground has been broken, and tests may not be able to show whether the new bone came from stem cells, rather than from the growth factor alone.
The operation put established techniques together, resembling a well-known experiment in which University of Massachusetts scientists grew a human ear using a mold on the back of a mouse in 1995, he said.
“If you put loads of blocks of bone mineral into a hole and you induce cellular activity by putting in growth factors, it’s a standard approach that people have used to induce the body’s own response,’’ said Brown, who was not connected with the study. “Clearly some of them are going to work and it sounds like for this patient, this has worked.’’
Biopsies of the jaw bone could later provide some answers on the quality of the bone, experts said.
“Just making the gross tissue shape right isn’t really the problem,’’ Brown said. “It’s what the shape of the tissue is at the microscopic and ultramicroscopic level. That’s the architecture which is so tricky and which is what gives function.’’
LANCET ABSTRACT:
BACKGROUND: A major goal of research in bone transplantation is the ability to avoid creation of secondary bone defects. We aimed to repair an extended mandibular discontinuity defect by growth of a custom bone transplant inside the latissimus dorsi muscle of an adult male patient. METHODS: Three-dimensional computed tomography (CT) scanning and computer-aided design techniques were used to produce an ideal virtual replacement for the mandibular defect. These data were used to create a titanium mesh cage that was filled with bone mineral blocks and infiltrated with 7 mg recombinant human bone morphogenetic protein 7 and 20 mL of the patient's bone marrow. Thus prepared, the transplant was implanted into the latissimus dorsi muscle and 7 weeks later transplanted as a free bone-muscle flap to repair the mandibular defect. FINDINGS: In-vivo skeletal scintigraphy showed bone remodelling and mineralisation inside the mandibular transplant both before and after transplantation. CT provided radiological evidence of new bone formation. Postoperatively, the patient had an improved degree of mastication and was satisfied with the aesthetic outcome of the procedure. INTERPRETATION: Heterotopic bone induction to form a mandibular replacement inside the latissimus dorsi muscle in a human being is possible. This technique allows for a lower operative burden compared with conventional techniques by avoiding creation of a secondary bone defect. It also provides a good three-dimensional outcome.